95% Deceptive: COVID Vaccine Efficacy & Medical Betrayal (Relative Deception Part I)
How statistical sleights of hand betrayed the heart and soul of medicine.
Note from the author: I am a self-employed private practice physician and independent researcher. Challenging medical hegemony is no easy task when going up against well-funded institutions with full-time staff and teams. It takes me dozens of hours to compile and publish this research. See end of this article for ways to support. In the meantime, stand up for medical sovereignty and the revelation of greater truth and subscribe now:
COVID Combat Zones
We are in the midst of informational and narrative warfare. All things COVID are active combat zones. Within this, vaccines are the most polarizing, controversial, hot button issue. If you have yet to check out Readers Aware: Rules of Engagement, please do so now.
On one extreme are those who believe COVID vaccines should be mandatory whether that is accomplished by: applying censorship, public shaming, and cancel culture to stifle dissent; making employment, school enrollment, travel, and private/public event participation contingent on vaccination status; threatening to remove licenses from medical professionals; or even going door-to-door with armed enforcers. (Yes, I have heard this suggested on multiple occasions.)
On the other extreme are those who believe COVID vaccines are a bioweapon being used for depopulation, soul-harvesting, and to socially engineer a technocratic, totalitarian, panopticon state.
Most people are in the center, doing their best to make sense of the risks and benefits of vaccination and early treatment options in order to make informed choices for themselves and their families. This post is intended to create more center, though I hope individuals at the extremes will also find value here.
Single-Pointed Focus
Given the complexity and vast nuance of the topic, this post is limited in scope to addressing a single issue: presenting COVID vaccine benefits using only a statistical measurement called relative risk reduction (RRR) is deceptive. It is more truth-full to present benefits using the absolute risk reduction (ARR). This is ubiquitously known by health authorities, institutions, and experts, but has been ignored by the dominant narrative.
Numbers Do Not Lie, but People Do
Numbers do not lie. Perhaps, but people do. And people use numbers – especially statistics – to persuade and deceive.

While we cannot know the intent of others, we can know the incentives that influence other beings and systems. The greater the incentives, the more probable it becomes that information is presented in a deceptive manner, and the more carefully you must look for the illusionist’s sleights of hand.
First Framer Advantage & Cascading Effects
On November 16, 2020 NIH announced “Promising Interim Results from Clinical Trial of NIH-Moderna COVID-19 Vaccine” reporting “the candidate was safe and well-tolerated and noted a vaccine efficacy rate of 94.5%.”1 The New England Journal of Medicine published the trial on February 4, 2021 where it reported “94.1% efficacy.”2
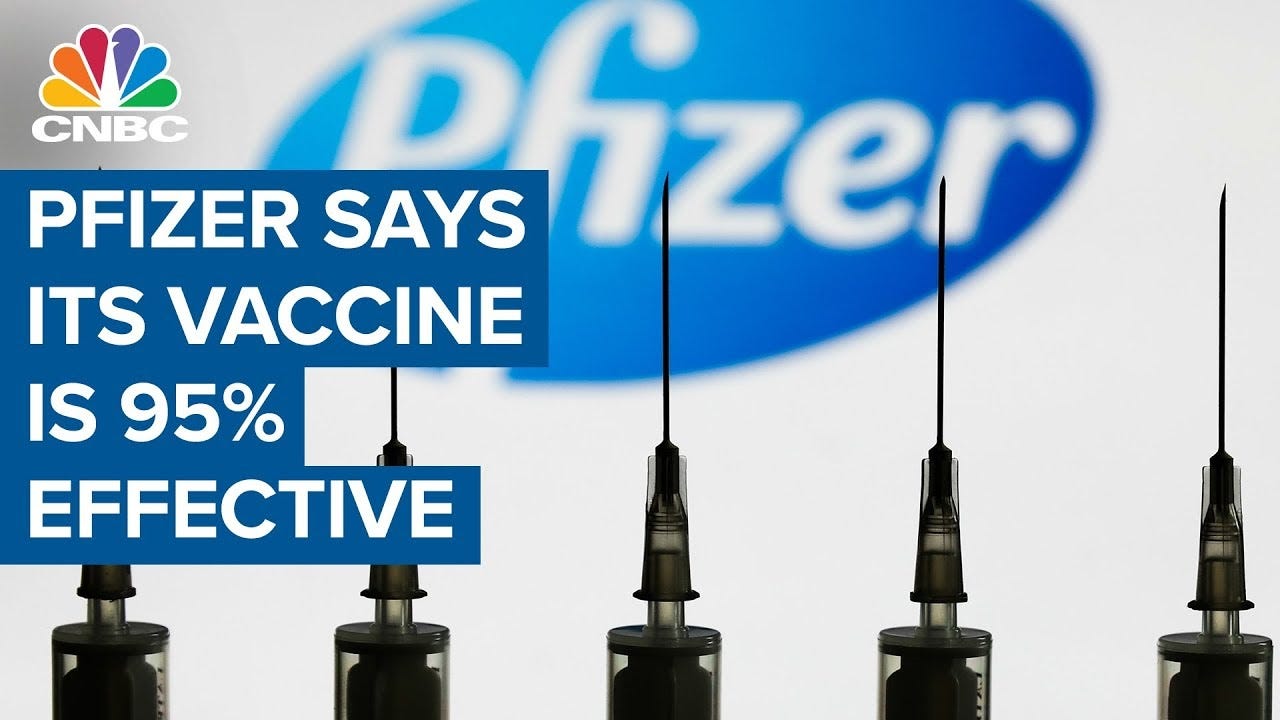
On December 10, 2020 Pfizer and BioNTech announced “Publication of Results from Landmark Phase 3 Trial of BNT162b2 COVID-19 Vaccine Candidate in The New England Journal of Medicine,” reporting “the vaccine candidate was well tolerated and demonstrated 95% efficacy in preventing COVID-19 in those without prior infection 7 days or more after the second dose.”3 The New England Journal of Medicine published the trial on December 31, 2020 reporting the vaccine was “95% effective in preventing Covid-19.”4
Media blitzkrieg ensued, hammering the “95% effectiveness” trope into the zeitgeist until it became the memetic anchor point for the global conversation on COVID vaccines. This initial frame, which clearly implies exceptional efficacy, in many ways continues to dominate the narrative.
There is a known first mover advantage in chess: white wins ~52-55% of the time in tournaments.5 I propose there is a similar phenomenon in strategic communications: whoever establishes the initial frame holds the edge in maintaining narrative dominance. This is especially the case when the initial frame is amplified asymmetrically by conglomerated media and ideologically-aligned social media platforms.
The net effect is many people understandably, but erroneously, concluded that COVID vaccines would reduce their risk of COVID by 95%.
“95% effective” is a powerful frame. It obviously implies exceptional efficacy, but it also communicates that the pharmaceutical companies have pulled off an extraordinary feat of biotechnological progress and medical science – and have done so in record time. This has compounding, cascading effects that increases people’s confidence, thereby increasing the likelihood that people buy into downstream claims with less skepticism. This in turn marginalizes dissent and reifies groupthink.
The reason for this, as far as I can ascertain, is along these lines: if the vaccine is so clearly effective, then it is foolish to question other claims about the vaccines.
I am paraphrasing what I have observed and experienced in both analog and digital spaces from the “95% effective” adherents. Exploring the merits or demerits is beyond the scope of this post (though I encourage you to leave a comment on which of these you would like to see explored in a future post).
From “95% effective” it is a short cognitive leap to:
When X% of the population vaccinates, COVID will (mostly) disappear
When COVID (mostly) disappears life will return to normal(-ish)
Vaccination protects the vulnerable
People have a social responsibility to vaccinate
The social contract means to participate in society you must vaccinate
Trials showed the vaccines are safe, therefore the vaccines are safe
The benefits of the vaccines clearly outweigh the risks
The unvaccinated are overburdening hospitals
If you do not vaccinate you are overburdening hospitals
Overburdening hospitals kills innocent people
The unvaccinated are the ones spreading COVID
If you do not vaccinate you are killing someone’s grandma or immunocompromised child
Trust the science, trust the experts
The unvaccinated are spreading misinformation
The unvaccinated are anti-science, brainwashed, delusional conspiracy theorists, ignorant, selfish assh*les
Anyone who questions vaccines should be shamed, censored, canceled, or penalized
Relative Deception
The “95% effective” frame comes from Pfizer-BioNTech’s published trial and refers to a specific statistical measurement called relative risk reduction, which indicates:
“how much the [intervention] reduced the risk of [a] bad outcome[ ] relative to the control group who did not have the [intervention].”6
In regards to this trial, what the relative risk reduction means is that the group receiving the vaccine had 95% fewer confirmed cases of COVID during the 2 months following vaccination when compared to the group that did not receive the vaccine.
Of note, the trials did not look at: the effectiveness of the vaccine on hospitalizations, deaths, or transmission; on the effect of confirmed cases of COVID beyond 2 months post-vaccination; safety beyond 2 months; in addition, the control group did receive vaccination in what is called “crossover” which makes medium and longer term safety data very difficult, if not impossible, to ascertain. Furthermore, for trial results to translate to real world conditions we must make at least two assumptions: that the population being vaccinated is comparable to the population in the study and that the virus does not evolve in a way that reduces vaccine effectiveness.
All of this sounds relatively benign. So why do I say using relative risk reduction as synonymous with effectiveness is deceptive?
Relative risk reduction is important information for clinicians and public health officials to know, but it is not useful in helping you as an individual make informed choices about your personal health. The reason for this is you must know your baseline risk in order for the relative risk reduction to be meaningful. A 99% reduction in risk of a rare event is unlikely to make a significant difference in your life, whereas a 1% reduction in risk of a common event may be more significant.
In fact, the relative risk reduction tells you nothing about how effective the vaccine will be in you. For this you need to know, at minimum, the absolute risk reduction, which accounts for baseline risk. And this is why using relative risk reduction to dominate a narrative and persuade people’s personal health choices is misleading and deceptive.
This is not just my opinion. This is not news. This is not a controversial supposition. It is well known by physicians, scientists, public health officials, medical journals, statisticians, and pharmaceutical companies.
Tell the Whole Truth
The whole truth is hidden in plain sight. Read the trials, get the data, and plug into straightforward calculations to get the absolute risk reduction. It is so simple even a Facebook fact checker can do it.
That is exactly what the authors of the article “COVID-19 vaccine efficacy and effectiveness—the elephant (not) in the room” did, which the Lancet published on April 20, 2021.7 All of the numbers below are quoted from this article, though I have reformatted for ease of presentation.
Keep in mind, the absolute risk reduction from these trials refers to the average decreased risk an individual has of getting a confirmed case of COVID (i.e. it does not confer information about hospitalization, death, transmission, nor “long COVID”) within a certain time window after vaccination.
Statistics are based on populations. They fall apart when applied to specific individuals. No statistic, no matter how good, will tell you how much an intervention will help or harm you. Absolute risk reduction is the best available measurement, but only conveys the average reduction in risk for the average individual in the trial.
Pfizer-BioNTech’s “95% effective” vaccine reduces risk on average by 0.84%
Moderna-NIH’s “94% effective” vaccine reduces risk on average by by 1.2%
Gamaleya’s “91% effective” vaccine reduces risk on average by 0.93%
J&J’s “67% effective” vaccine reduces risk on average by 1.2%
AstraZeneca–Oxford’s “67% effective” vaccine reduces risk on average by 1.3%
As you can clearly see, there is no correlation between the espoused effectiveness of a vaccine based on its relative risk reduction, and how much the vaccine decreases your personal risk of a confirmed case of COVID based on absolute risk reduction.
Given the COVID vaccines reduce an individual’s risk of a confirmed case within a certain time window after vaccination by 0.84-1.3% – which some people will consider a marginal benefit – obvious questions ensue.
Do these effect sizes warrant public shaming, censorship, cancellation, and threatening the livelihoods of the unvaccinated? Do these effect sizes warrant vitriol and venom towards the unvaccinated for interpreting the risks-benefits differently than the dominant narrative?
Do these effect sizes warrant the kinds of draconian measures towards the unvaccinated that are now commonplace (see: Australia)?
How confident are we – in the absence of medium and long term safety data – that the potential medium and long term risks of the vaccines are less than 0.84-1.3%?
How does this vastly different presentation of benefits affect people’s personal health choices? How likely are you to get a vaccine when it is advertised as “95% effective” versus you are told it reduces your risk by 0.84%?
While there are many people (“bulls”) who would get the vaccine regardless of the effect size (including those who see vaccination as an act of social responsibility rather than a personal health choice), it is likely that a lot more “undecideds” would opt out.
This is one of the reasons why the whole truth was not being told.
Absolutely Clear: Authorities, Institutions, and Experts Already Knew This
In 2010, the appropriately named CONSORT group, which stands for Consolidated Standards of Reporting Trials, released “Updated Guidelines for Reporting Parallel Group Randomized Trials.”
According to the Annals of Internal Medicine, which published the statement, “The CONSORT … statement is used worldwide to improve the reporting of randomized, controlled trials.”8 In an effort to promote widespread dissemination, the CONSORT statement was also published in the “BMJ, The Lancet, Obstetrics & Gynecology, PLoS Medicine, Open Medicine, Journal of Clinical Epidemiology, BMC Medicine, and Trials.”9
According to the CONSORT group, the CONSORT statement “is an evidence-based, minimum set of recommendations for reporting randomized trials. It offers a standard way for authors to prepare reports of trial findings, facilitating their complete and transparent reporting, and aiding their critical appraisal and interpretation.”10
The statement is currently endorsed by 585 journals, which is “over 50% of the core medical journals listed in the Abridged Index Medicus on PubMed.”11 The list of endorsers includes the New England Journal of Medicine who published both the Moderna-NIH and Pfizer-BioNTech vaccine trials.
Within one of the statement’s tables, it states (albeit in small font so perhaps the New England Journal of Medicine missed it):
“presentation of both absolute and relative effect sizes is recommended”12
Now, I concede this is a softly worded recommendation. Perhaps the editors at the New England Journal of Medicine interpreted this along the lines of a suggested wine pairing rather than as the evidence-based recommendations coming from the mostly widely publicized set of standards for randomized controlled trials that their very own journal endorsed.
But this is just the opinion of one organization. What do other health authorities have to say on the topic of relative risk versus absolute risk reduction?
In August 2011, the FDA published a 242-page document titled “Communicating Risks and Benefits: An Evidence-Based User's Guide.” It clearly states (emphases mine):
“when information is presented in a relative risk format, the risk reduction seems larger and treatments are viewed more favorably than when the same information is presented using an absolute risk format.”13
It then asks the question, “What general practical advice [for communicating risks and benefits] can the science support?” It unambiguously recommends:
“Provide absolute risks, not just relative risks. Patients are unduly influenced when risk information is presented using a relative risk approach; this can result in suboptimal decisions. Thus, an absolute risk format should be used.”14
Earlier that same year, the Cochrane Library (whose motto is “Trusted evidence. Informed decisions. Better health.”), published a systematic review titled “Using alternative statistical formats for presenting risks and risk reductions,” its numerous findings included (emphases mine):
“In terms of presenting risk reduction … clinicians are more impressed by the bigger numbers of the relative changes than by the smaller absolute changes for the same results. In addition, absolute terms offer physicians more concrete information about an intervention because they are based on both the magnitude of the reduction of risk and the baseline risk. Relative terms may thus be misleading because they ignore the baseline risk.”
“relative risk reduction (RRR) resulted in 21% more participants deciding to take statins… compared to the absolute summary statistics suggesting that people are more likely to be persuaded when presented with a relative summary statistic”
“[People] perceived interventions to be more effective … and were more persuaded to prescribe or accept an intervention … when exposed to RRR compared to ARR and NNT… Overall there were no differences between health professionals and consumers ... This would be of concern because health professionals play a key role in medical decision making. It also suggests that the formal education and training of health professionals apparently has no effect on their handling of statistical information.”15
The authors of the Cochrane review concluded:
“For communicating risk reductions, relative risk reduction (RRR), compared with absolute risk reduction (ARR) and number needed to treat (NNT), may be perceived to be larger and is more likely to be persuasive… it is uncertain whether presenting RRR is likely to help people make decisions most consistent with their own values and, in fact, it could lead to misinterpretation.”16
From the U.S. Preventive Services Task Force’s, “General Principles for Making Recommendations” (emphasis mine):
“In judging the magnitude of benefit, absolute reductions in risk matter more than relative risk reductions.”17
Now, if these heavy hitters are not sufficient to demonstrate that absolute risk reduction is intellectually more honest than relative risk reduction, consider these additional references from research literature.
On September 27, 2003, the British Medical Journal published two different articles regarding the communication of medical risks.
“Strategies to help patients understand risks,” stated:
“Use absolute numbers; do not use relative risks”18
And “Simple tools for understanding risks: from innumeracy to insight,” stated (emphases mine):
“Confusion caused by relative risks can be avoided by using absolute risks... However, health agencies typically inform the public in the form of relative risks. Health authorities tend not to encourage transparent representations… report[ing] benefits in relative rather than absolute risks because the numbers look larger.”19
From the 2008 textbook, Smart Health Choices: Making Sense of Health Advice (emphasis mine):
“Absolute risk reduction… is the most useful way of presenting research results to help your decision-making.”20
On October 5, 2011, the Journal of the National Cancer Institute published, “Helping Patients Decide: Ten Steps to Better Risk Communication,” their number two recommendation was:
“Present Statistical Information Using Absolute Risk Rather Than Using Relative Risk or Number Needed to Treat Formats”21
It further stated (emphases mine):
“research has consistently shown… that changes in risk appear larger when presented using relative risk than when using an absolute risk and that the treatments were viewed more favorably when presented in terms of relative risk. This use of relative risk information can inappropriately lead patients to believe that a treatment is more effective than what has been empirically proven. Additionally, several studies have found that medical students and practicing physicians were more likely to recommend treatment (eg, chemotherapy) if the information was presented using relative risks (compared with absolute risks or NNT). Given these findings, we strongly recommend that risk information be consistently presented to patients using absolute risks.”22
The journal PM&R published, “Communicating Risks Clearly: Absolute Risk and Number Needed to Treat,” on March 21, 2012. It said (emphases mine):
“Researchers have an obligation to present risks as fairly and clearly as possible for their readers. However, they typically favor the most obscure presentation: relative risks. Relative risks can be misleading, because a dramatic reduction in relative risk may correspond to only a small drop in absolute risk.”
“Absolute and relative risks convey very different pictures of the effect of an intervention or exposure. Readers and researchers should pay more attention to absolute risks and the related statistic, the number needed to treat (or to harm). Absolute risks are more informative and straightforward than relative risks; they are also useful for assessing the overall harms and benefits of an intervention”23
From “Common pitfalls in statistical analysis: Absolute risk reduction, relative risk reduction, and number needed to treat,” published in Perspectives in Clinical Research in 2016 (emphases mine):
“Physicians tend to overestimate the efficacy of an intervention when results are expressed as relative measures rather than as absolute measures. ARR … is probably a more useful tool than RRR to express the efficacy of an intervention. Thus, reporting of absolute measures is a must.”24
From “Relative risk versus absolute risk: one cannot be interpreted without the other,” published on February 27, 2017 in Nephrology Dialysis Transplantation (emphases mine):
“Relative risks have… [a] major weakness, that the underlying absolute risks are concealed and readers tend to overestimate the effect when it is presented in relative terms… absolute risk gives a better representation of the actual situation and… often give[s] more relevant information.”
“the sole reporting of relative risks has a major drawback… it may obscure the magnitude of the effect of an intervention. When relative risks are used for the presentation of effects of a treatment, this can make the treatment seem better than it actually is. For example, investigators may claim that a certain treatment reduces mortality by 50% when the intervention reduces death rates from 0.002% to 0.001%, an improvement the clinical relevance of which may be questioned.”25
In 2018, the American Academy of Family Physicians published in their journal Family Practice Management, “Five Ways to Communicate Risks So That Patients Understand,” which stated (emphasis theirs):
“USE ABSOLUTE RISK RATHER THAN RELATIVE RISK TO REDUCE BIAS … Research has shown that changes in risk appear larger when presented using relative risk versus absolute risk. And a more recent systematic review demonstrated that data presentations that included absolute risks maximized accuracy without influencing decisions to accept therapy.
Based on these findings, because the same information can be communicated either way, using absolute risk is important if you do not want to unduly influence the patient's decision.”26
In response to the article, the medical editor of the journal said (emphasis mine):
“It turns out that we as physicians have some bad habits. We tend to overestimate the risk of a condition and underestimate the risk of treatment. Additionally, we often present differences in risk as relative risk rather than absolute risk. This can be misleading. For example, if X cuts your risk of Y by 50 percent, that sounds compelling. But it could mean reducing your risk of Y from, say, 40 percent to 20 percent, or it could mean reducing your risk of Y from 2 percent to 1 percent. I don't know about you, but I'd be much less likely to take on the risk of a treatment to receive an absolute risk reduction of 1 percent as opposed to an absolute risk reduction of 20 percent.”27
Quoting again from “COVID-19 vaccine efficacy and effectiveness—the elephant (not) in the room,” published by the Lancet on April 20, 2021, it stated (emphasis mine):
“Vaccine efficacy is generally reported as a relative risk reduction (RRR)... ARRs tend to be ignored because they give a much less impressive effect size than RRRs”28
It is absolutely clear that authorities, institutions, and experts already know that relative risk reduction increases the perception of benefit and biases towards intervention. They already know that absolute risk reduction is the superior measurement for accurately conveying the benefits of an intervention, and that it must be presented.
In other words, if your incentive is to maximize profits from a medical intervention, put the relative risk reduction front and center (and omit the absolute risk reduction).
Omission is Betrayal
There are bold-faced lies, there are white lies, and there are lies of omission.
Reporting relative risk reduction without the absolute risk reduction is a lie of omission.
Telling the whole truth and nothing but the whole truth requires reporting the absolute risk reduction.
This is the ethical standard if the actual desired outcome is informed consent. Informed consent is fundamental to autonomy and sovereignty. Anything short of this standard is unethical. Therefore, whenever relative risk reduction is reported in isolation, the actual desired outcome is manufacturing consent. Know this, and you will forever see through the statistical sleight of hand of the illusionists.
For health professionals and institutions to feign ignorance of this deception, and continue to willfully perpetuate it, borders on malfeasance. It is professional misconduct. It is abandonment of patients and the public. It is indicative of the widespread decay within the institutions entrusted to guide us. It deteriorates the sanctity of informed consent. It is unethical. It pollutes the epistemic commons. It is an act of warfare.
It is a betrayal of the heart and soul of medicine.
Show your support: Stand up for medical sovereignty and the revelation of greater truth. Subscribe to this Substack, follow on social media, connect me personally with strategic podcasts, blogs, and influencers, share this content, and offer a donation. Humanity and our future generations thanks you.
Donate: PayPal
Facebook @ Benjamin Kaplan-Singer (most active)
Twitter @thesovereignmd
Instagram @thesovereignmd
LinkedIn @ Dr. Benjamin Kaplan-Singer
https://www.nih.gov/news-events/news-releases/promising-interim-results-clinical-trial-nih-moderna-covid-19-vaccine
https://www.nejm.org/doi/full/10.1056/nejmoa2035389
https://www.pfizer.com/news/press-release/press-release-detail/pfizer-and-biontech-announce-publication-results-landmark
https://www.nejm.org/doi/full/10.1056/nejmoa2034577
https://en.wikipedia.org/wiki/First-move_advantage_in_chess
https://www.ncbi.nlm.nih.gov/books/NBK63647/
https://www.thelancet.com/journals/lanmic/article/PIIS2666-5247(21)00069-0/fulltext
https://www.acpjournals.org/doi/10.7326/0003-4819-154-4-201102150-00016
Ibid
http://www.consort-statement.org/
http://www.consort-statement.org/about-consort/endorsers1
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2857832/pdf/1745-6215-11-32.pdf
https://www.fda.gov/files/about%20fda/published/Communicating-Risk-and-Benefits---An-Evidence-Based-User%27s-Guide-%28Printer-Friendly%29.pdf
Ibid
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6464912/
Ibid
https://www.uspreventiveservicestaskforce.org/uspstf/about-uspstf/methods-and-processes/procedure-manual/procedure-manual-section-7-formulation-task-force-recommendations
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC200818/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC200816/
https://www.ncbi.nlm.nih.gov/books/NBK63647/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3218625/
Ibid
https://onlinelibrary.wiley.com/doi/full/10.1016/j.pmrj.2012.01.001
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4763519/
https://academic.oup.com/ndt/article/32/suppl_2/ii13/3056571
https://www.aafp.org/fpm/2018/1100/p28.html#fpm20181100p28-b8
https://www.aafp.org/fpm/2018/1100/p4.html#fpm20181100p4-b1
https://www.thelancet.com/journals/lanmic/article/PIIS2666-5247(21)00069-0/fulltext




BTW, great article on BPC157 and NO on PubMed for early treatment of Covid. Check it out
https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC8575535/#__ffn_sectitle
If i understand your article correctly, you're pointing out that the absolute risk reduction is lower because COVID is rare?
If so, does that analysis change in the face of Omicron, which appears to be very common?